Mental health is an essential component of individual and collective well-being, yet access to mental health services remains uneven and inadequate in many parts of the world. From long waiting lists to high costs and social stigma, numerous barriers prevent people from seeking or receiving the care they need. In the face of growing mental health crises, especially after the compounded stress of the COVID-19 pandemic, a new model for accessible, inclusive, and community-centered care is gaining traction: transforming local community centers into hubs for mental health resources. These familiar neighborhood institutions, traditionally known for hosting recreational classes or public meetings, are uniquely positioned to become safe, stigma-free spaces where individuals can access mental health education, support services, and therapeutic resources.
The Mental Health Gap and Why Community Matters
Despite increasing awareness about mental health, a significant gap persists between those who need care and those who receive it. According to the World Health Organization, nearly one in eight people globally live with a mental health condition, but fewer than half get the appropriate support. Factors such as geographic location, lack of insurance, cultural stigma, and fear of discrimination prevent people from accessing traditional clinical care. In response, experts and activists are increasingly turning to community-based solutions that are rooted in trust, familiarity, and accessibility. Community centers—already integrated into the daily lives of many residents—represent a natural extension of this shift. They are not only physically accessible but also symbolically open, welcoming people from all walks of life without the formality or intimidation often associated with clinical settings.
Destigmatizing Mental Health Through Visibility and Education
One of the most powerful roles community centers can play is in normalizing mental health discussions. When workshops on managing anxiety or group sessions on coping with grief are held in the same buildings as dance classes or senior lunches, mental health becomes part of the everyday fabric of life rather than an isolated issue. Visibility leads to normalization. A mother attending a parenting workshop might feel more comfortable later signing up for a stress-reduction session. A teenager taking a coding class might discover a peer-led mental health group in the next room. By embedding mental health into a broader slate of programs, community centers help chip away at stigma, particularly in cultures or generations where discussing emotions is taboo. These centers can also serve as venues for public campaigns, film screenings, and art exhibits that explore mental health themes, further opening the door for conversations and curiosity.
Providing Accessible Services Without the Red Tape
Traditional mental health care often involves navigating insurance requirements, long intake processes, and complex appointment systems. Community centers, by contrast, can offer lower-threshold services—drop-in counseling sessions, walk-in support groups, or informal check-ins with peer mentors. These services may be offered in partnership with local clinics or universities, bringing trained professionals or supervised interns directly into the neighborhood. For people experiencing mild to moderate mental health challenges—such as stress, grief, loneliness, or life transitions—these community-based interventions can be sufficient and transformative. For those with more acute needs, the community center can function as a triage and referral point, helping individuals connect with more intensive care through trusted guidance and support. In either case, the emphasis is on removing bureaucratic and psychological barriers to care.
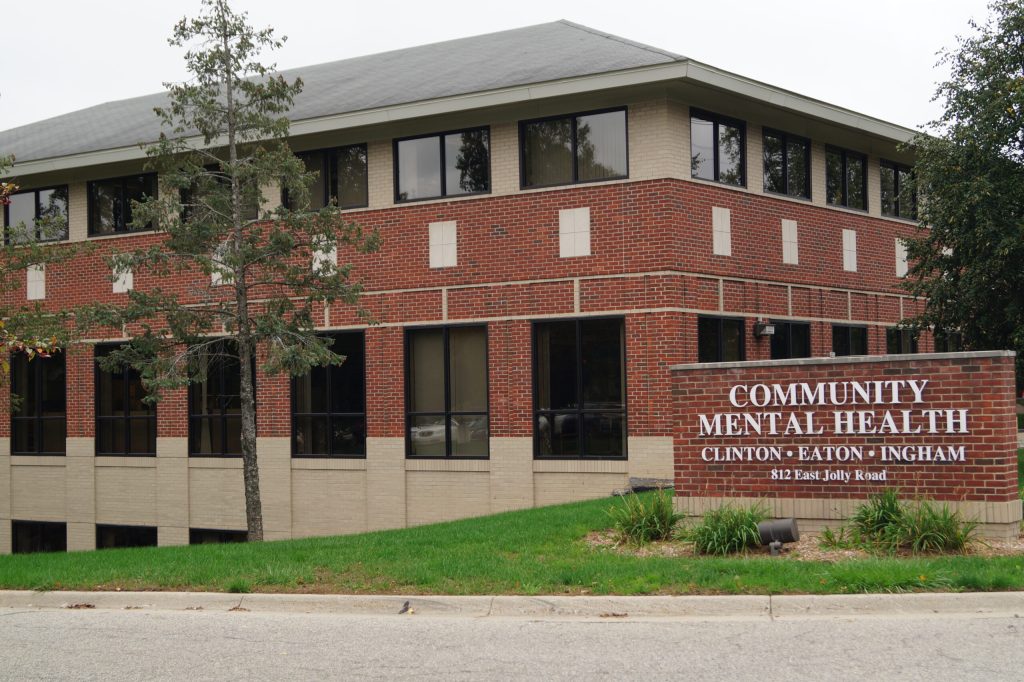
Serving the Underserved: Equity and Inclusion
Community centers are often located in areas that are historically underserved by healthcare systems—urban neighborhoods, rural towns, and lower-income communities. As such, they are ideally positioned to reduce disparities in mental health access. By offering services at little or no cost, in multiple languages, and with cultural sensitivity, these centers ensure that care is not limited to those with financial means or specific cultural capital. Programs can be tailored to the unique needs of specific populations: support groups for LGBTQ+ youth, parenting workshops for immigrant families, mindfulness sessions for veterans, or trauma-informed yoga for survivors of violence. The key is flexibility and community involvement. When programs are co-created with the populations they serve, they are more likely to be relevant, respectful, and effective.
Peer Support and Community Connection
A distinguishing feature of community-based mental health services is the central role of peer support. Unlike clinical models that often focus on top-down treatment, peer-led initiatives emphasize mutual aid, shared experience, and collective resilience. A community center might host recovery circles, mental health storytelling events, or peer counseling programs where trained individuals with lived experience of mental health challenges support others navigating similar journeys. This model not only expands the available workforce for mental health support but also builds community cohesion. The message is clear: you are not alone. In spaces where people can be both givers and receivers of support, healing becomes a shared endeavor rather than a solitary struggle. These relationships, rooted in empathy and equality, can be just as powerful as professional interventions.
Integrated Wellness: Mental Health in Context
Mental health does not exist in isolation. It intersects with housing, employment, food security, and physical health. Community centers, with their holistic approach to services, are well-positioned to address mental health within this broader ecosystem. For example, a mental health program might be paired with job training, a community meal, or an exercise class. Nutrition workshops can include content on the gut-brain connection. Financial literacy seminars can address the anxiety of debt. This integrative model respects the complexity of people’s lives and avoids reducing mental health to a narrow clinical diagnosis. Instead, it supports people in the context of their lived realities—celebrating strengths, building skills, and fostering hope. When a person comes to a community center, they don’t just get a service—they get a network.
Designing Mental Health-Friendly Spaces
The physical environment of a community center plays a critical role in its effectiveness as a mental health hub. Thoughtful design can communicate safety, warmth, and inclusivity. Natural lighting, calming color palettes, comfortable seating, and private areas for confidential conversations are small elements that make a big difference. Programming areas should be easily navigable, with clear signage and welcoming staff. Artwork, posters, and literature should reflect the diversity of the community and promote messages of resilience and support. Quiet rooms or sensory spaces can be designated for those who need a break from overstimulation. These design choices signal that the space values mental well-being not just in programming but in every detail of the environment.
Partnerships and Sustainability
To sustain their role as mental health hubs, community centers must build strong partnerships with mental health professionals, local health departments, nonprofits, and educational institutions. These collaborations can bring funding, training, and expertise into the center while allowing service providers to reach community members more effectively. Universities may offer student interns, clinics may rotate therapists into onsite sessions, and public health agencies may use the center as a site for outreach or data collection. Sustainability also depends on stable funding, staff development, and community input. Grants, donations, and government support are vital, but so is accountability to the people the center serves. Regular feedback loops, community advisory boards, and participatory planning processes ensure that mental health initiatives remain relevant, inclusive, and rooted in real needs.
Success Stories and Evidence of Impact
Across the globe, examples abound of community centers leading the way in mental health innovation. In Toronto, the Centre for Addiction and Mental Health partners with local community hubs to offer culturally adapted counseling and education. In Los Angeles, the Boyle Heights Arts Conservatory uses creative expression and mentorship as tools for youth mental health empowerment. In Nairobi, community health workers use mobile apps within local centers to screen and refer people for mental health support. Evaluations of these programs consistently show positive outcomes: reduced stigma, increased service uptake, improved well-being, and greater trust in mental health services. More importantly, they reflect a shift from mental health as a medical issue to mental health as a community value.
Empowering Communities, Transforming Futures
The mental health crisis cannot be solved by professionals alone. It requires the full engagement of communities—neighbors, teachers, faith leaders, parents, and youth—working together to create supportive environments where emotional well-being is a shared priority. Community centers, by virtue of their accessibility, flexibility, and rootedness, are ideal platforms for this collective care. They remind us that healing does not always happen in a therapist’s office. Sometimes, it begins in a room filled with laughter, storytelling, music, and shared meals. Sometimes, it starts when someone walks through the door and sees a flyer that says, “You’re not alone.” As we envision more equitable and compassionate models of mental health care, we would do well to start with the spaces closest to home—the community centers that already hold the hearts of our neighborhoods.