For centuries, the human body was understood through separate systems—digestive, nervous, immune, and so on. But modern science is unraveling a much more complex and interconnected story, especially when it comes to our mental health. At the heart of this discovery lies a two-way communication system between the gut and the brain, known as the gut-brain axis. It turns out that what happens in your digestive tract doesn’t just impact bloating or bowel movements—it can influence your mood, emotional stability, cognitive clarity, and even your risk for anxiety and depression. In short, a healthy gut is essential for a healthy mind, and a balanced diet is one of the most powerful ways to support both.
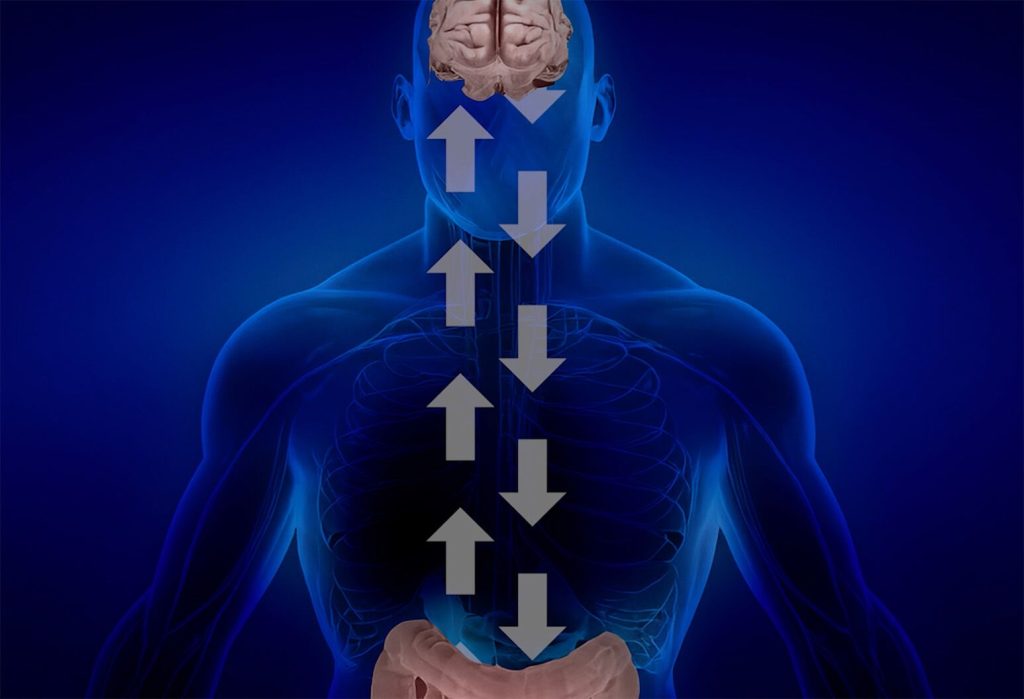
Understanding the Gut-Brain Axis
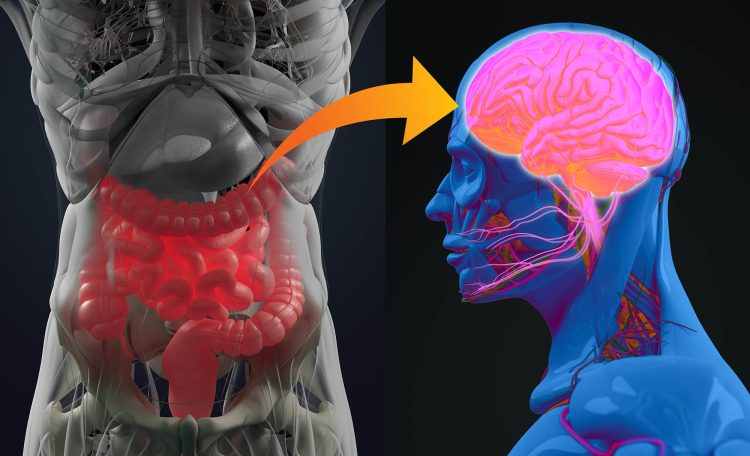
The gut-brain axis refers to the bidirectional communication network that links the central nervous system (CNS), which includes the brain and spinal cord, with the enteric nervous system (ENS), often referred to as the “second brain” located in the gastrointestinal tract. This intricate system operates through neural pathways, hormones, and most importantly, the microbiome—a vast community of trillions of microorganisms living in the intestines.
These gut microbes produce neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA), which directly affect mood and cognition. Surprisingly, about 90% of serotonin, the “feel-good” neurotransmitter, is produced in the gut. Disruption in this communication system—due to inflammation, infection, stress, or a poor diet—can negatively impact brain function, emotional balance, and overall mental health.
The Role of the Microbiome in Mental Health
The microbiome is now considered a key player in the brain’s ecosystem. A diverse and balanced microbial population supports a healthy immune system, regulates inflammation, and helps synthesize essential nutrients and brain chemicals. When the microbiome is thriving, it sends positive signals to the brain that can enhance mood, sharpen focus, and reduce anxiety.
Conversely, dysbiosis—an imbalance in the gut microbiota—has been linked to various mental health disorders, including depression, generalized anxiety, bipolar disorder, and even neurodevelopmental conditions such as autism. Dysbiosis may increase gut permeability (often called “leaky gut”), allowing harmful substances like lipopolysaccharides (LPS) to enter the bloodstream. This can trigger systemic inflammation and neuroinflammation, both of which are strongly associated with mood disorders.
Inflammation: The Hidden Link Between Diet and Depression
One of the central mechanisms connecting poor diet to mental health issues is inflammation. A diet high in sugar, processed foods, and unhealthy fats can promote chronic low-grade inflammation throughout the body—including the brain. This inflammation can interfere with neurotransmitter signaling, damage neural pathways, and increase the risk of depression and cognitive decline.
On the other hand, anti-inflammatory diets rich in whole foods, fiber, healthy fats, and antioxidants help reduce oxidative stress and promote neurogenesis (the growth of new brain cells). Mediterranean-style diets, in particular, have been extensively studied for their protective effects on mental health. Such diets emphasize fruits, vegetables, legumes, whole grains, fish, and extra virgin olive oil—all of which support gut health and emotional stability.
Probiotics and Fermented Foods: Fueling the Mind Through the Gut
Probiotics are live bacteria that, when consumed in adequate amounts, confer health benefits by enhancing the gut microbiome. These beneficial bacteria can modulate the immune system, improve digestion, and influence neurotransmitter production. Clinical trials have shown that probiotic supplementation can alleviate symptoms of anxiety, depression, and stress.
Fermented foods such as yogurt with live cultures, kefir, miso, kimchi, sauerkraut, and tempeh are natural sources of probiotics. Including these in your diet can improve microbial diversity and resilience. Studies suggest that individuals who regularly consume fermented foods report lower levels of social anxiety and emotional distress.
Prebiotics: Feeding Your Gut’s Good Bacteria
Just as important as introducing beneficial bacteria is feeding them well. Prebiotics are types of dietary fiber that nourish the good bacteria already residing in your gut. Foods rich in prebiotics include garlic, onions, leeks, asparagus, bananas, apples, oats, and Jerusalem artichokes. These foods help maintain a thriving and balanced microbiome, which in turn supports the gut-brain connection.
Prebiotic fiber is also involved in the production of short-chain fatty acids (SCFAs) like butyrate, which help strengthen the gut lining, reduce inflammation, and support brain health. A diet low in fiber deprives gut microbes of their preferred fuel, leading to reduced SCFA production and a less effective gut-brain link.
Blood Sugar Balance and Emotional Stability
What you eat also affects your blood sugar, and stable blood sugar is essential for emotional regulation. High-sugar, high-carb meals can cause blood sugar spikes followed by crashes, leading to irritability, fatigue, and mood swings. These rapid fluctuations in energy can mimic symptoms of anxiety and depression, making it hard to distinguish emotional issues from dietary responses.
Eating balanced meals with protein, fiber, and healthy fats slows digestion and prevents blood sugar rollercoasters. Whole grains, legumes, vegetables, lean meats, nuts, and seeds form the foundation of a stabilizing diet. Avoiding excessive caffeine and alcohol also helps maintain mood equilibrium.
Essential Nutrients for Gut and Brain Harmony
Several key nutrients play dual roles in maintaining both gut and brain health. Deficiencies in these nutrients are common and often overlooked in mental health evaluations:
- Omega-3 Fatty Acids: Found in fatty fish (like salmon, sardines, and mackerel), flaxseeds, and walnuts. These reduce inflammation and support brain cell membrane integrity.
- Magnesium: Found in leafy greens, nuts, seeds, and legumes. Helps regulate the nervous system and supports serotonin production.
- Zinc: Abundant in pumpkin seeds, chickpeas, and shellfish. Important for immune function and neurotransmitter activity.
- Vitamin D: Produced from sunlight and found in fortified foods and fatty fish. Low levels are linked to depression and seasonal affective disorder.
- B Vitamins (especially B6, B9, and B12): Found in whole grains, leafy greens, and animal products. They help produce brain chemicals and reduce homocysteine levels, which are associated with depression when elevated.
A diet lacking in these essential nutrients can impair both gut function and emotional well-being. In some cases, supplementation under medical supervision may be necessary to restore balance.
The Impact of Stress and Emotional Eating
It’s important to recognize that diet and mental health influence each other in both directions. While food affects mood, mood also affects food choices. Stress, anxiety, and sadness can drive cravings for sugary, fatty, and processed comfort foods. These foods may provide short-term relief but often worsen gut health and contribute to long-term mental distress.
Mindful eating practices, including slowing down during meals, chewing thoroughly, and tuning into hunger and fullness cues, can reduce emotional eating and improve digestion. Combining these habits with stress-reducing techniques such as deep breathing, yoga, or walking can help regulate the gut-brain axis and promote long-term wellness.
Building a Gut-Friendly, Mood-Boosting Diet
Creating a diet that supports both your gut and your brain doesn’t require perfection—just a shift in priorities. Here’s how to start:
- Prioritize Plant-Based Diversity: Aim for a wide variety of vegetables, fruits, legumes, nuts, and seeds to increase fiber and microbial diversity.
- Incorporate Fermented Foods Daily: Add a serving of yogurt, kefir, kimchi, or tempeh to your meals regularly.
- Choose Whole Grains Over Refined Carbs: Brown rice, oats, and quinoa support stable blood sugar and provide prebiotic fiber.
- Eat Healthy Fats: Use olive oil for cooking, snack on nuts, and enjoy fatty fish a few times per week.
- Reduce Sugar and Processed Foods: These disrupt the microbiome and increase inflammation.
- Stay Hydrated: Water supports digestion and cellular function, and dehydration can negatively affect mood and cognition.
- Cook More at Home: Homemade meals tend to be higher in fiber, nutrients, and good fats—and lower in inflammatory ingredients.
The Future of Mental Health: Integrating Nutrition and Psychiatry
The idea that mental health care should include dietary advice is gaining ground. Psychiatrists, therapists, and general practitioners are beginning to acknowledge the profound influence of nutrition on mood and cognitive performance. Nutritional psychiatry, though still emerging, is already changing lives by offering a complementary approach to medication and therapy.
As research continues to illuminate the gut-brain connection, future mental health strategies will likely be more holistic, integrating gut-supporting nutrition, stress management, physical activity, and personalized care. For now, the science is clear: food is a foundational pillar of emotional well-being. And your gut—far more than just a digestive organ—is a vital partner in your mental health journey.